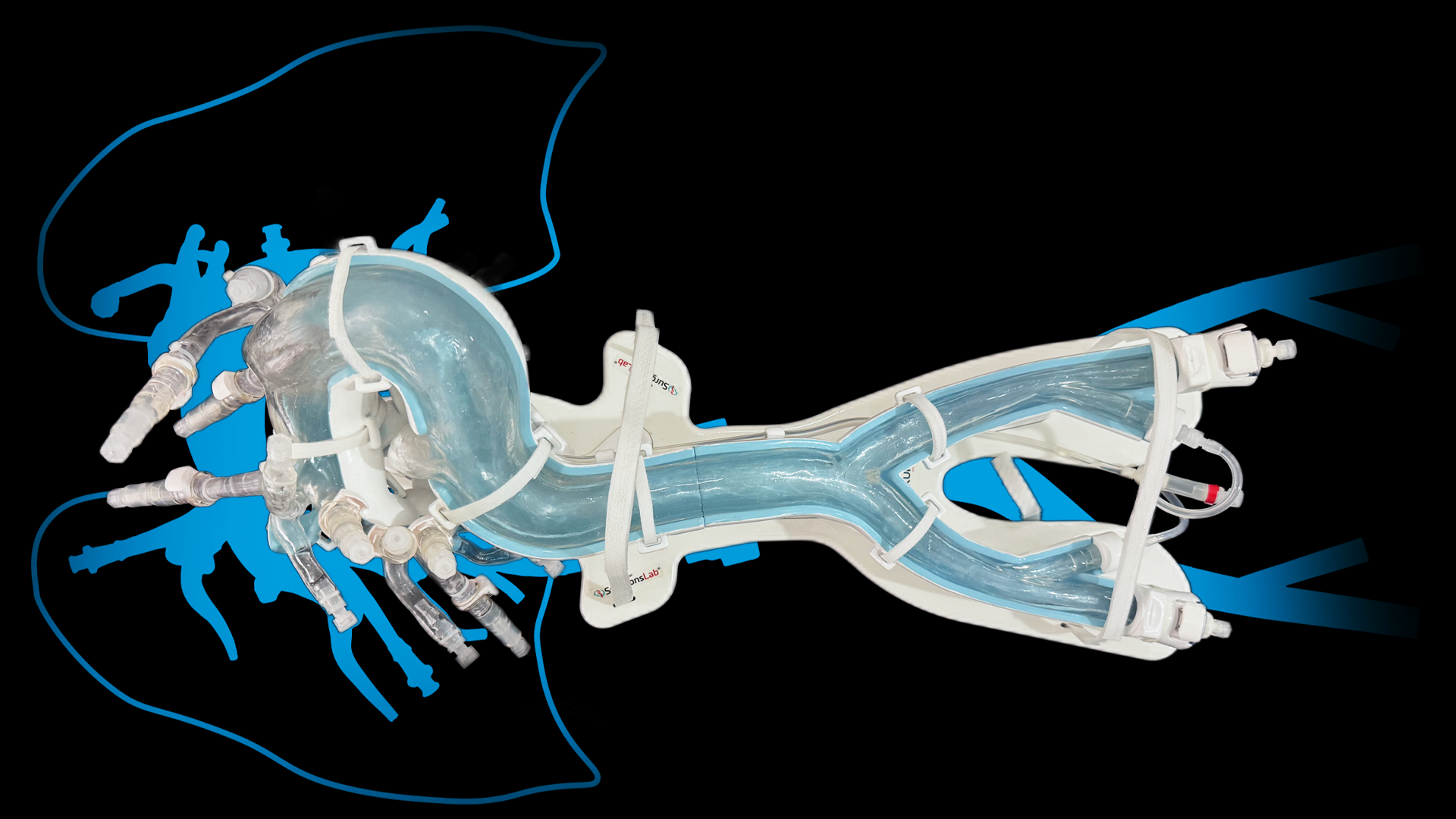
Catheterization | DVT-CAVT Simulation Technique
Our bench-top and full-scale Pulmonary Embolism models offer customizable, closed-loop systems that closely replicate real-world conditions. Models can demonstrate the Deep Vein Thrombosis (DVT) to Computer Assisted Vacuum Thrombectomy (CAVT) technique on our realistic endovascular simulation model, designed for training and procedural testing.
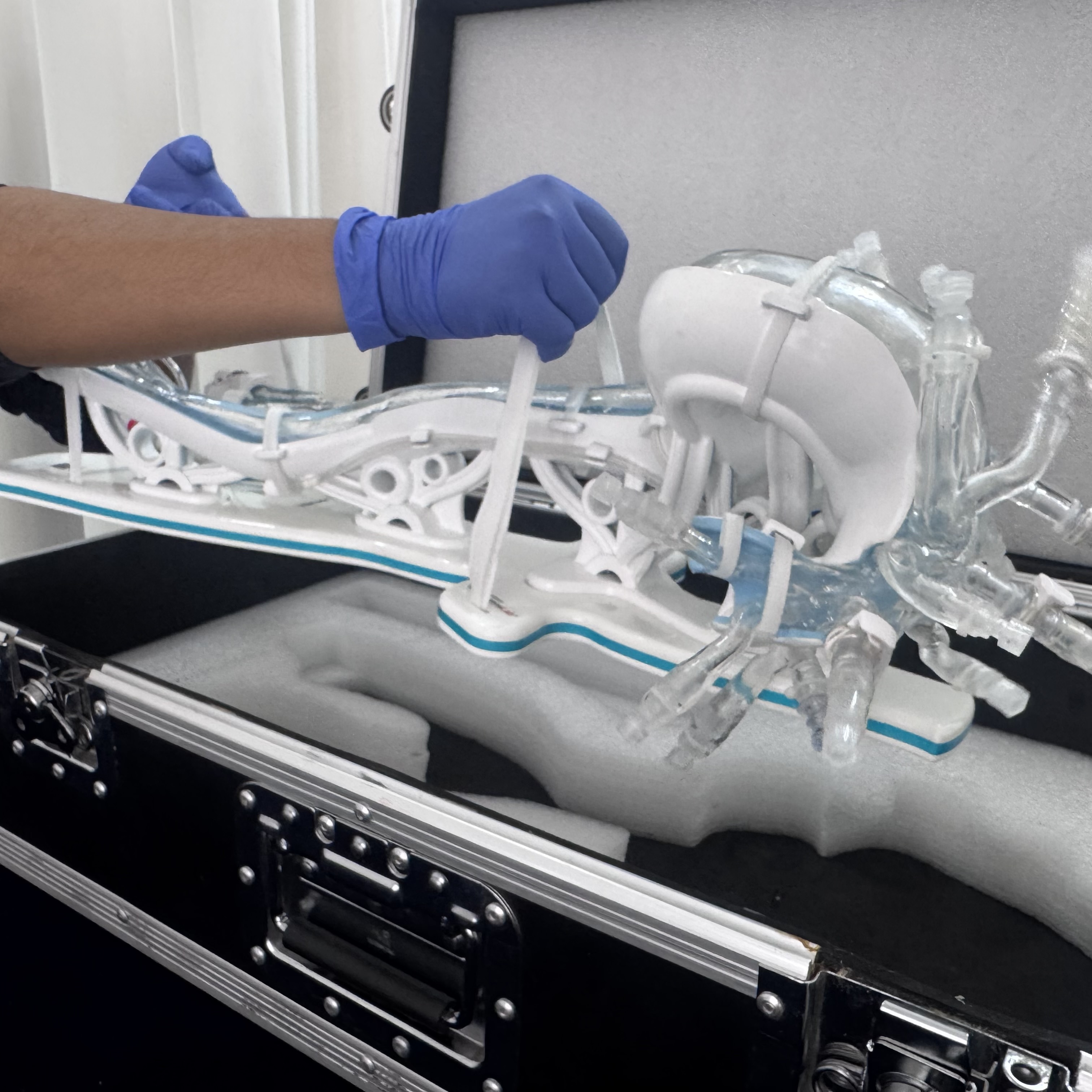
Showcase how effectively your catheter minimizes blood loss in the simulation model !

These are the most commonly asked questions. can't find what you are looking for use our chatbot.